Take a break from doing nothing and do less
The default mode network, mindfulness, and you
I.
You’re exercising in your garage. A friend who lives down the street drops by. While chatting, you ask him to hand you a 15-pound dumbbell sitting by his feet.
He can’t pick it up. “Whatever,” he laughs. “Why do you want to lift a piece of metal over and over? Seems pointless.”
II.
Next time you get the chance (or now), close your eyes and pay attention to your breath for two minutes straight. Feel the air entering and leaving your lungs. If something else pulls your attention away — a memory, a catchy song, a train of thought, a sound from outside — bring it back to your breath and restart the clock.
When people try this and realize how hard it is, many react like the friend in the garage. After all, weightlifters are at least visibly active. Meditation, while difficult, seems like doing less than nothing. You’re neither thinking hard about something nor letting your mind wander.
So why does meditating for hours a day turn the monks who do it into walking factories of good vibes and present-moment awareness, like bodybuilders who clearly lift? And why are the rest of us like spindly-armed weaklings, barely able to spend two minutes, let alone twenty, alone with our breath? If the gains are real, where do they come from?
III.
In 1874, a doctor in Liverpool named Richard Caton discovered that the brains of rabbits and monkeys had electric current running through them. The current would dramatically change when he shone lights in their eyes and when they slept. It disappeared when they died.
In hindsight, this seems like an obvious thread to pull. At the time, it was a quirky novelty. It took fifty years for someone to discover the same thing in humans.
The German psychiatrist who did so in 1924, Hans Berger, waited five years to publish his results. He feared he’d be ridiculed for them, having no formal training in electrical engineering. He was. After five more years, though, other scientists reproduced his work and EEG — short for electroencephalography, literally meaning “electric head writing” — began its journey to becoming one of neuroscience’s most important tools.
One of his observations was that the human brain shows significant EEG activity even when it isn’t engaged in any particular task. Evidence for this claim mounted, but was more or less ignored, throughout the 20th century.
Finally, in the 1990s, neuroscientists began to use fMRI scanners, which measure blood flow to specific regions of the brain. Participants waiting around between experiments, their minds wandering, would show not just brain activity, but brain activity in a consistent set of regions.
In 2001, this set of regions got its name from Dr. Marcus Raichle and his team at Washington University in St. Louis: the default mode network, or DMN.
Far from being background noise, the DMN has been found to be a crucial system in the brain. Malfunctions and abnormalities in it show up in every mental illness you can shake a stick at, including ADHD, anxiety, Alzheimer’s, depression, OCD, Parkinson’s, PTSD, schizophrenia, and more.
IV.
If mind-wandering is the DMN’s bread and butter, then rumination — mind-wandering in an obsessive and/or negative way — would be its “soda and ice cream.” Rumination is the calling card, the signature, of a hyperactive DMN. The word’s original meaning refers to when goats and cows regurgitate grass to chew on it, which is apt.
It’s also a core symptom of depression and anxiety. These two illnesses have spread like wildfire over the last two years, with the percentage of young American adults showing symptoms almost quadrupling. Recent stresses like COVID-19 have been the spark, but the kindling has been accumulating.
Humans didn’t evolve for a lot of things we now deal with. We didn’t evolve for the way social media shows us the successes and not the failures of our acquaintances, or the way it bombards us with the worst headlines from around the world every day. We didn’t evolve for the way modern jobs disconnect us from the fruits of our labor, encouraging our bosses to claim arbitrary amounts of it. I won’t get into a pie chart of reasons for our faulty DMNs. The point is, they’ve been in hot water for a while now.
Some ancient humans had depression, anxiety, and faulty DMNs too. There are genetic predispositions for these disorders and we had to get them from somewhere. But there’s ample evidence that, by and large, their DMNs operated at a happy medium instead of churning so constantly that many of them avoided being alone with their thoughts. Quite the opposite.
And so, just as moving your body in certain ways can prevent repetitive strain injury, or brushing your teeth can prevent tooth decay, mindfulness — even though it looks like doing less than nothing — can give us a layer of armor against the stresses of modern life, and the “soda and ice cream” of rumination, pushing us back toward this happy medium.
Let’s cut to the chase already. How does it do so? The most explanation you’ll get from many pop science books, like How to Change Your Mind and Altered Traits (both of which are still great), is “too much default network bad, mindfulness good.” I wanted to dig deeper.
V.
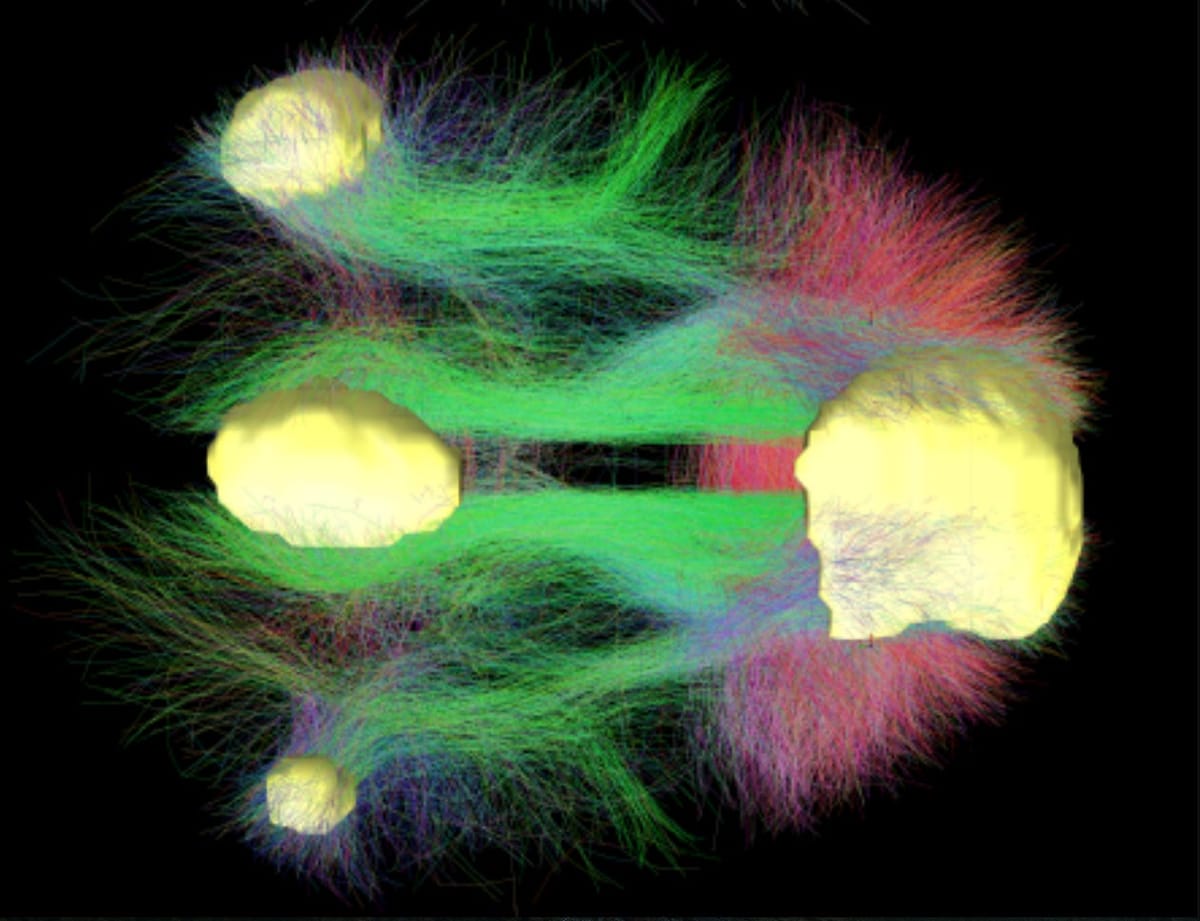
In 2011, a neuroscientist named Dr. Vinod Menon published a paper outlining what he called the “triple network model” of mental disorders. The interactions of three particular brain networks, he argued, do the lion’s share of work in causing and explaining a wide swath of mental illnesses. One is the DMN. The other two are the central executive network (CEN) and the salience network (SN).
The CEN is a taskmaster and is most active during activities that make you concentrate and hold things in memory — math problems, memorization, and triaging orders as a barista, to name a few. Meanwhile, the SN scans your environment, emotions, and thoughts for important (“salient”) things, switching other networks off and on to deal with them as needed.
In a healthy brain, the main hubs of the DMN are “anti-correlated” with those of the CEN and SN. This means they’re connected, but when one is activated, the other isn’t. For the CEN or SN to be fully “on,” the DMN should become less active, and vice versa.
Mindfulness, then, by being an “on switch” for the CEN and SN, is a reliable “off switch” for the DMN. In meditation, your CEN holds your attention on something; your SN watches it, but also stays on the lookout for mind-wandering; when your SN notices that, it kicks your CEN into gear, letting you consciously concentrate on that thing again. Repeat.
Activities besides meditation activate your CEN and SN, too. And things besides exercise can use your muscles. Meditation, however, like spending time at the gym, is special; it’s the serious, repetitive, targeted way to improve the underlying machinery. Two key hubs of the CEN and SN, the dlPFC (dorsolateral prefrontal cortex) and dACC (dorsal anterior cingulate cortex) respectively, show especially pronounced changes in long-term meditators. We’ll come across these again.
Within a few weeks of meditating daily — and you’ll feel yourself getting better at it in that time, like a drummer more easily getting “in the pocket” — you’ll find you have more control over where your attention goes and when. This applies to your thoughts and environment (athletes and gamers take note) but also your emotions.
Your wandering mind will feel less “sticky” overall, less compulsive. Thoughts and emotions that used to be hard to let go of won’t seem that way so much anymore.
The extra attention you have from not being so caught up in them, ruminating on them, can now be used to reappraise them, act on them. This is especially helpful when what you’re perceiving is negative, as the news around us increasingly is.
VI.
It’s time for a brief reality check. Working out helps prevent, but doesn’t fix, a torn ACL. Brushing teeth helps prevent, but doesn’t fix, an abscess. Meditation helps prevent, but doesn’t fix, severe depression. There’s a reason psychiatrists treat suicidal patients with pills and not by telling them to meditate.
When DMNs become hyperactive, parts of them undergo the opposite of what happens in meditation. They start to “eat” parts of other networks, becoming more positively correlated with them, instead of anti-correlated as is normal.
This hurts those networks’ effectiveness. It becomes harder for them to turn off the DMN, which gets more hyperactive, and so on in a vicious cycle. Your SN and CEN begin working more in the service of your ruminating thoughts, rather than against them, rerouting your attention back to them, treating their negativity more like physical pain signals from your environment.
Feedback loops like these, laid over things like pre-existing genetic factors, traumatic life experiences, and addictions (even mild ones), can do severe damage over time, and not just to whole-brain networks but to specific regions in ways that meditation can’t fix in any reasonable amount of time.
In depression specifically, one hub of the DMN called the vmPFC (ventromedial prefrontal cortex) tends to malfunction, along with nearby regions like the sgACC (subgenual anterior cingulate cortex). This area is heavily involved in processing emotional signals from the midbrain, and is also a hotspot of serotonin receptors. (A paper I read mentioned a subject who attempted suicide with a crossbow; against all odds, he survived with a lesion in his vmPFC that cured his depression, though it also crippled his emotional decision-making skills.)
Through mechanisms that scientists are still fleshing out, burning out those receptors with too much DMN activity can cause hyperactive processing of negative emotions and hypoactive (under-active) processing of positive ones. This, in turn, can lead to things like anhedonia (loss of pleasure), a pervasive feeling of dread and hopelessness, and suicide.
Chemical interventions — SSRIs like Prozac and other medications — are often the only way forward given the patient’s state. Once the pills start working, the patient is better equipped to do the grueling long-term work — therapy, exercise, habitual emotional regulation — that keeps serotonin around and normalizes the wiring of all three big networks.
What if there was a treatment that took both approaches at once, chemical and cognitive, and also took a small fraction of the time?
VII.
I recently came across a Twitter thread in which someone described the cognitive effects of LSD, commonly known as acid, and this particular tweet leapt out at me.
What Garcia is describing here sounds remarkably similar to a brain whose CEN and SN are allowed to work in the absence of DMN interference.
This is, in fact, what’s happening. LSD and similar compounds like psilocybin have been combined with therapy to create highly effective treatments for many mental illnesses, especially ones heavily involving the DMN.
These drugs are potent serotonin agonists, meaning they mimic serotonin and can fit into many of the brain’s serotonin receptors. Flooding the brain with them essentially “crashes” the DMN for hours.
Dr. Robin Carhart-Harris, a leading researcher of how these drugs work, has found that in the hours and days after psychedelic therapy sessions, the DMN comes back with reconfigured patterns of activity. Especially for people with mental illness, these new patterns much more closely resemble those of healthy brains; single sessions of this kind of therapy have shown results comparable to weeks upon weeks of traditional therapy with SSRIs.
This kind of therapy remains widely illegal.
I live near the University of Wisconsin in Madison, another leader in the field of psychedelic research. Meanwhile, the state itself has unusually strict drug laws, especially compared to neighbors like Illinois and Michigan. This is absurd. There is no need for this to be a partisan issue, and if people in red counties could see what these new treatments can do for mental illness and addiction, which don’t spare people based on political leanings, then they may think differently about them.
Of course, there are other interesting leads on the horizon. A new-ish technology called transcranial magnetic stimulation (TMS) can directly influence neural oscillations (the things that show up in EEG) and have proven effective in treating depression. We’re also finding evidence that the oscillations controlling our breathing may interact much more directly than we thought with other ones in our prefrontal cortex, hinting at benefits of meditation we didn’t know about.
Unfortunately, it’s to the advantage of capital — pharmaceutical companies who want to sell their existing wares and not so much new and harder-to-patent treatments that can be taken far less often — for it to stay this way. There will be casualties.
VIII.
In a recent study, watching personalized videos on TikTok was found to have roughly the opposite effect of mindfulness, despite technically anchoring the user in the present moment. It activates another DMN hub, heavily involved both in social cognition and self-focused thought, called the dmPFC or dorsomedial prefrontal cortex, along with the brain’s reward centers.
This region is near, and highly connected to, the vmPFC. Like the vmPFC, it can cause serious problems if it’s too active and its connections go awry. If it “goes rogue,” becoming hyperconnected to the rest of the frontal DMN, it can contribute too much to self-focused thought and become worse at regulating emotion, one of its key jobs.
As a rare place in the brain where all three big networks meet, the dmPFC can also become less capable of helping to switch between other networks; TikTok compounds this problem by deactivating key hubs of the CEN and SN elsewhere in the brain, like the dlPFC and dACC mentioned earlier.
We have let millions of teenagers plug themselves into a spring-loaded rumination machine for hours a day, setting up their brain networks for lifelong domination by the DMN. We teach few of them about the benefits of mindfulness, and continue to outlaw therapies best situated to help them overcome intractable mental illness. Politicians blame things on mental health like mass shootings that aren’t truly about that and then don’t even do anything about mental health.
Just as scientists who neglected the brain’s resting state to focus on task-based activity have held back our understanding of the brain for decades, we today, neglecting our default mode networks, keep our own mental health in the dark and in jeopardy.
The science is here. The solutions are right in front of us. What are we doing?
Less than nothing, and not in a good way.
References
III.
- Electroencephalography on Wikipedia
- Default mode network on Wikipedia
IV.
- OECD statistics on depression and anxiety increases
- Rumination and the default mode network: Meta-analysis of brain imaging studies and implications for depression
- The default network and self-generated thought: component processes, dynamic control, and clinical relevance
V.
- Large-scale brain networks and psychopathology: a unifying triple network model
- Functional connectivity of default mode network components: Correlation, anticorrelation, and causality
- Spectral dynamic causal modeling of mindfulness, mind-wandering, and resting-state in the triple network using fMRI
- Meditation experience is associated with differences in default mode network activity and connectivity
- Mindfulness is associated with intrinsic functional connectivity between default mode and salience networks
- Effects of Meditation Experience on Functional Connectivity of Distributed Brain Networks
- Trait Mindfulness and Functional Connectivity in Cognitive and Attentional Resting State Networks
- Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators
- Disrupting The Resting State: Meta-Analytic Evidence That Mindfulness Training Alters Default Mode Network Connectivity
VI.
- Depression is associated with hyperconnectivity of an introspective socio-affective network during the recall of formative relationship episodes
- Distinct Regions of Prefrontal Cortex Mediate Resistance and Vulnerability to Depression
- Depression, rumination and the default network
- Depressive Rumination, the Default-Mode Network, and the Dark Matter of Clinical Neuroscience
- Experience sampling during fMRI reveals default network and executive system contributions to mind wandering
- Functional connectivity changes with rapid remission from moderate-to-severe major depressive disorder
- The effects of antidepressant treatment on resting‐state functional brain networks in patients with major depressive disorder
- Top-down control of serotonin systems by the prefrontal cortex: a path towards restored socioemotional function in depression
- Resting-State Functional Connectivity of Subgenual Anterior Cingulate Cortex in Depressed Adolescents
- The Subgenual Anterior Cingulate Cortex in Mood Disorders
- Cognitive behavioral therapy for depression changes medial prefrontal and ventral anterior cingulate cortex activity associated with self-referential processing
VII.
- Psilocybin for treatment-resistant depression: fMRI-measured brain mechanisms
- Psilocybin-assisted mindfulness training modulates self-consciousness and brain default mode network connectivity with lasting effects
- Functional connectivity of the anterior cingulate cortex predicts treatment outcome for rTMS in treatment-resistant depression at 3-month follow-up
- Organization of prefrontal network activity by respiration-related oscillations
- A Bridge between the Breath and the Brain: Synchronization of Respiration, a Pupillometric Marker of the Locus Coeruleus, and an EEG Marker of Attentional Control State
VIII.
- Viewing personalized video clips recommended by TikTok activates default mode network and ventral tegmental area
- Resting-state functional MRI in depression unmasks increased connectivity between networks via the dorsal nexus
- Increased prefrontal cortex connectivity associated with depression vulnerability and relapse
- Individual differences in dispositional mindfulness and brain activity involved in reappraisal of emotion
- Rumination and Default Mode Network Subsystems Connectivity in First-episode, Drug-Naive Young Patients with Major Depressive Disorder
- The role of the subgenual anterior cingulate cortex in dorsomedial prefrontal–amygdala neural circuitry during positive‐social emotion regulation
- Prefrontal cortex and depression
- A treatment-resistant default mode subnetwork in major depression
- Default mode network dissociation in depressive and anxiety states




